Since I have Crohn’s disease, this article really stuck out
at me. After reading it, I don’t think the findings are very definitive, but
this may lead to more research on the mechanism of how the normal flora gets
shifted in the intestines of Crohn’s disease patients.

Since I have Crohn’s disease, this article really stuck out
at me. After reading it, I don’t think the findings are very definitive, but
this may lead to more research on the mechanism of how the normal flora gets
shifted in the intestines of Crohn’s disease patients.
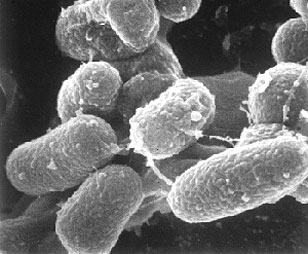
This study tested aerosols and biofilm samples from the
River Taff area in Cardiff, Wales. 5 aerosol samples and 30 domestic shower
samples from 23 homes across 4 UK counties were collected with a high volume
impaction sampler, along with biofilm samples from shower tubes and heads. Epifluorescence
microscopy, bacterial cultures, and polymerase chain reaction assays were
performed on each of these samples. Mycobacterium avium subspecies paratuberculosis
was detected in 1 of the 5 river samples and 3 of the 30 shower samples across
all regions.
This study concluded that the exposure to this organism
could be due to aerosols from the rivers and domestic showers. This led them to
the associated of aerosols in the river taff influencing human Crohn’s Disease.
I have never been to Wales or the UK so I cannot speak on my
exposure to this organism, but I am glad to see research in finding possible
causative agents.
Article Reference: Bacteria linked to Crohn's disease found in shower, river water aerosols
